Human papillomavirus (HPV)-negative head and neck squamous cell carcinoma (HNSCC) has remained challenging to treat, particularly due to its resistance to conventional therapies and limited response to immunotherapy. However, a recent study conducted by researchers at the Medical College of Wisconsin sheds new light on a potential breakthrough in this arena. Their findings, published in Translational Oncology, highlight the untapped potential of T cells within HNSCC tumors and pave the way for more effective immunotherapeutic strategies.
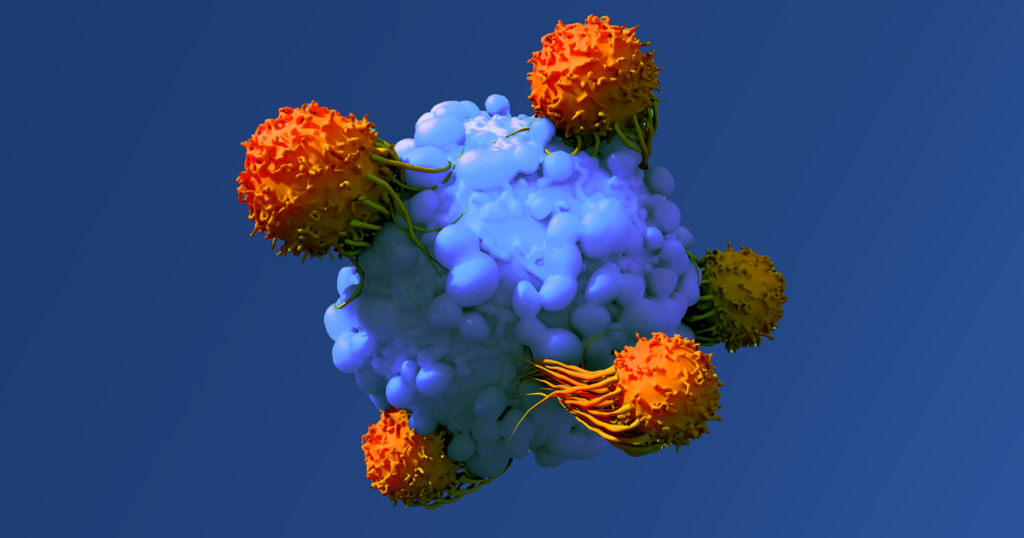
One of the primary barriers to successful immunotherapy in HNSCC lies in the dysfunctional nature of T cells within the tumor microenvironment. While it’s known that these T cells exhibit phenotypic dysfunction, questions lingered regarding their actual functional capacity and ability to target and kill tumor cells effectively.
To address this gap in knowledge, the researchers employed Bruker’s cutting-edge optofluidic and proteomic barcoding platforms to evaluate the functionality of T cells in HNSCC.
Using Bruker’s proteomic barcoding platform, the researchers investigated whether TILs (tumor-infiltrating lymphocytes) from recurrent HNSCC retained functional capacity despite adverse clinical characteristics. Remarkably, they found that these TILs not only expanded and retained a central memory phenotype but also demonstrated potent effector and chemotactic immunogenicity upon T cell receptor stimulation ex vivo. This suggests that even in treatment-resistant disease, TILs possess rescuable functional capacity, offering hope for novel therapeutic interventions.
Additionally, Bruker’s optofluidic platform allowed for the identification of cancer-specific T cells at the single-cell level across HNSCC patients. By co-culturing patient-matched TILs with malignant cells, the researchers were able to visualize individual tumor-killing T cells and confirm their role in inducing tumor cell death. This groundbreaking approach provides valuable insights into the immune-mediated mechanisms underlying tumor cell killing and opens avenues for personalized immunotherapies tailored to individual patients.
This study emphasizes the importance of combinatorial approaches in tackling HNSCC. While anti-PD1 therapy alone proved insufficient to reinvigorate TILs clinically, the observed functional potential of these T cells suggests that combination therapies may hold the key to overcoming treatment resistance and improving patient outcomes.
“Our autologous tumor cell-T cell platform delivers the most rigorous methodology to-date to identify immunogenic tumor-specific T cells in HNSCC. This work lays the foundation for personalized tumor-specific TCR and neoantigen discovery.” This represents a significant step forward in the quest to conquer HNSCC and underscores the transformative power of immunotherapy in the fight against cancer.”
Looking ahead, the findings from this study not only deepen our understanding of T cell functionality in HNSCC but also offer promising prospects for cancer-specific TCR and neoantigen discovery. By leveraging these innovative platforms, researchers can identify and harness the full therapeutic potential of T cells, paving the way towards more effective and personalized treatments for HNSCC patients.
If you’re ready to learn how Bruker’s platforms can help you develop more effective immunotherapeutic strategies, get in touch with one of our experts.