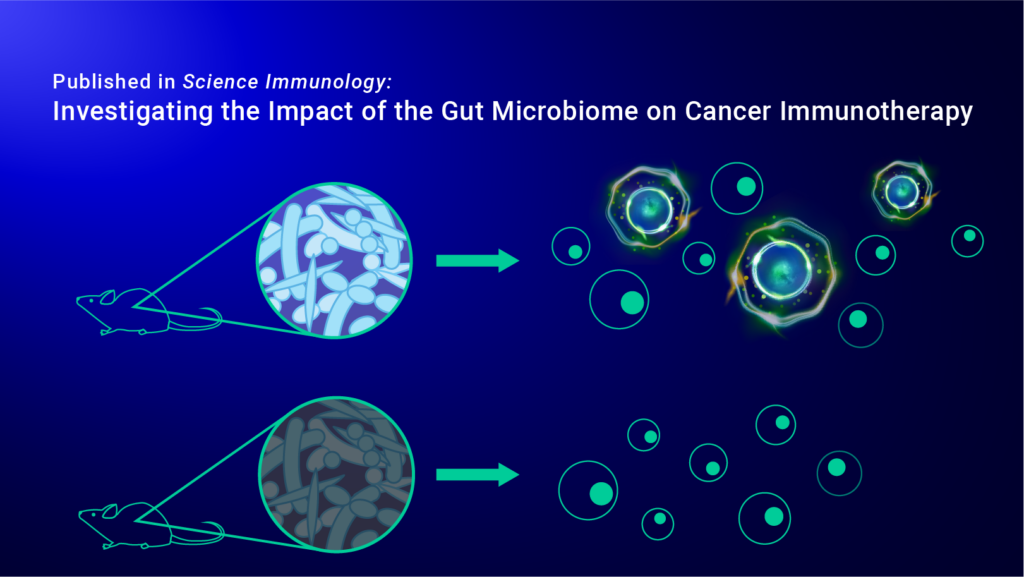
Immune checkpoint inhibitor therapy (ICT) is a form of cancer immunotherapy that specifically targets immune checkpoint regulators that tumor cells use to evade immune responses. Though ICT treatments have shown promising results in patients with previously “incurable” cancers, up to 50% of patients continue to remain unresponsive to the therapy. To identify the mechanisms driving this contrast between patient response, researchers are investigating a variety of host-associated factors that could be causing this discrepancy, such as the gut microbiome.
The gut microbiome is the collection of microorganisms, including bacteria, that live within the digestive tract. In previous studies, researchers found that gut microbiota could play an important role in modulating cancer immunotherapies, specifically ICT treatments, but the underlying mechanisms were unclear. Understanding how the gut microbiota augments and promotes anticancer immune responses is essential to improving the therapeutic response of ICT treatments in patients. By using the IsoCode® Single-Cell Secretome and CodePlex® platforms, researchers were able to investigate the complex relationship between the gut microbiome and cancer immunotherapy efficacy.
Immune Checkpoint Blockade Initiates Anti-Cancer Response through Gut Microbiota Stimulation
In a recent study published in Science Immunology, researchers at the University of Texas Southwestern Medical Center investigated the relationship between the gut microbiome and the efficacy of cancer immunotherapies by identifying distinct signatures of the gut microbiota in a preclinical melanoma mouse model treated with a combination therapy of PD-1/CTLA-4 immune checkpoint blockade. Immediately after treatment, the researchers noticed a significant enrichment of bacteria in the mesenteric lymph nodes and tumor, prompting them to then identify whether these bacteria could activate immune function. By stimulating the immune cells from the mouse models with bacterial lysates, the researchers found that the bacteria activate immune stimulatory phenotypes in the immune cells. Further experiments to relate the gut microbiome to ICT efficacy showed that dendritic cells facilitated gut bacteria translocation into lymphoid organs during PD-1/CTLA-4 treatment.
Since antibiotics have previously been shown to be associated with poorer outcomes in patients receiving ICT, the researchers also wanted to investigate the effect of antibiotics on the response rates of ICT treatment. Using IsoCode® Single-Cell Secretome and CodePlex® platforms, the researchers evaluated changes in immune function following antibiotic treatment in both CD8+ T cells and dendritic cells. Dendritic cell supernatants analyzed using the CodePlex platform showed a marked decrease in multiple cytokine secretions following antibiotic depletion of endogenous gut bacteria. At a single-cell level, the researchers found that antibiotic use decreased CD8+ T cell polyfunctionality and effector function, which are both significant contributors to anti-tumor responses. These results directly link gut microbiome health to the immune response and the efficacy of immune checkpoint therapy.
Using Single-Cell Functional Analysis to Identify Key Drivers of Immunotherapy Efficacy
With Bruker Cellular Analysis’ suite of single cell analysis tools, researchers can investigate the relationships between cancer immunotherapy treatment and patient outcomes. Polyfunctionality has been associated with increased clinical response to numerous therapy types, including ICT and CAR-T therapy, and continue to guide the development of advanced medicine. By understanding how the gut microbiome is related to the efficacy of combination therapies, researchers can continue to develop stronger, more effective treatments for difficult diseases.